
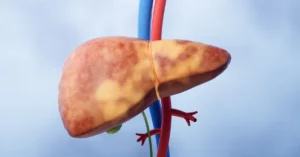
Fatty Liver Disease
Fatty liver disease, once a rare condition, has now become

Acute liver failure is a severe and life-threatening condition characterized by the rapid loss of liver function, typically occurring within days or weeks. Unlike chronic liver diseases that develop gradually over months or years, acute liver failure strikes suddenly and requires immediate medical attention. The quick deterioration of liver function in this condition leads to serious complications such as encephalopathy (brain dysfunction), coagulopathy (blood clotting disorders), and potential multi-organ failure. Understanding the definition of acute liver failure is essential for recognizing the urgency and severity of this condition, as it demands prompt and aggressive treatment to prevent fatal outcomes.
Here are key aspects of acute liver failure:
Recognizing the symptoms and understanding the urgency of acute liver failure are critical steps in ensuring timely and effective treatment, potentially including liver transplantation, to save lives.
Acute liver failure is a rapid and severe condition characterized by the sudden onset of symptoms such as jaundice, confusion, and fatigue. Recognizing these symptoms early is crucial for timely intervention and effective treatment.
The causes of acute liver failure are diverse, ranging from viral infections and drug toxicity to autoimmune disorders and genetic conditions. Understanding these causes is crucial for timely diagnosis, effective treatment, and improving patient outcomes.
Acute liver failure progresses rapidly, making it crucial to recognize its stages to ensure timely medical intervention. Each stage presents specific symptoms and challenges, and understanding these can help in identifying acute liver failure before it becomes life-threatening. The progression typically follows three main stages:
Acute liver failure treatment is crucial for stabilizing the patient and preventing further complications. The approach to treatment varies depending on the underlying cause and the stage of the condition. Early and aggressive intervention is essential to improve outcomes.
Preventing acute liver failure involves taking proactive steps to protect your liver from damage and addressing potential risk factors before they lead to severe conditions. By following a healthy lifestyle and being mindful of the causes of liver damage, you can significantly reduce your risk of developing acute liver failure. Here are some effective strategies to help prevent this serious condition:
Acute liver failure is not only a severe condition on its own but also a precursor to various life-threatening complications. These complications arise rapidly, often requiring immediate medical attention to prevent further deterioration. The swift onset of acute liver failure complications highlights the importance of early diagnosis and intervention.
These complications underscore the need for immediate and comprehensive acute liver failure treatment to prevent irreversible damage and improve survival rates.
Liver transplantation is often the only viable treatment for acute liver failure, especially in advanced stages where other treatments fail. The eligibility for a liver transplant is determined by several critical factors to ensure the success of the procedure and the long-term health of the patient. Here are the key criteria for transplant eligibility:
These criteria are essential to ensure that liver transplantation is the best option for treating acute liver failure and that the patient has the best chance for a successful recovery.
Acute liver failure is a critical condition that demands prompt and effective treatment. Early recognition of symptoms, understanding the causes, and knowing the stages of acute liver failure can save lives. If you or someone you know is at risk, it is essential to seek medical attention immediately. Timely intervention, including the possibility of a liver transplant, is key to surviving acute liver failure.
Liver failure can develop rapidly, sometimes within just 48 hours, depending on the cause. Conditions like acute liver failure progress swiftly, making early detection and treatment crucial.
Yes, liver damage can occur suddenly, especially in cases of acute liver failure. This sudden onset requires immediate medical intervention to prevent life-threatening complications.
No, survival without a liver is impossible. The liver performs essential functions, and in cases of liver failure, a transplant may be the only option for survival.
The prognosis varies, but without treatment, acute liver failure can be fatal within days. With timely treatment, including potential liver transplantation, survival rates improve significantly.
The signs of liver failure include jaundice, confusion, fatigue, swelling, nausea, and an increased tendency to bruise or bleed. Recognizing these signs early can be critical for treatment.

Fatty liver disease, once a rare condition, has now become
Cirrhosis of the liver is a serious medical condition that




Undergoing a liver transplant is a monumental step in treating

A liver transplant is a crucial and intricate surgical procedure

Embarking on a liver transplant journey in India is a

Embarking on a liver transplant journey in India is a profound and transformative decision, necessitating thorough preparation for the best results. From the initial evaluation to grasping eligibility criteria, every step is crucial