
Fatty Liver Disease
Fatty liver disease, once a rare condition, has now become
A liver donor is a person who voluntarily donates a portion of their healthy liver to a recipient in need of a liver transplant. This can be done either through a deceased donation or, increasingly, through a living liver donation. In a Living Donor Liver Transplant, the donor is alive and well, offering a portion of their liver to someone whose liver is failing due to conditions such as cirrhosis, liver cancer, or other liver-related diseases.
To become a living liver donor, an individual must meet strict medical and psychological criteria to ensure their safety and the success of the transplant.
Key points about a liver donor include:
A liver donor plays a crucial role in saving lives, and their donated liver portion regenerates to full size within months. Living liver donation not only helps reduce waiting times for recipients but also provides a more immediate, healthier transplant option. This selfless act offers both a second chance at life for the recipient and a sense of fulfillment for the donor.
Becoming a liver donor is a significant decision that requires careful consideration, both emotionally and medically. To ensure the safety of both the donor and recipient, potential donors must meet strict health and eligibility criteria for a Living Donor Transplant. The health and well-being of the donor are of utmost importance, as liver donation is a major surgery.
Key criteria for living liver donation include:
In addition to meeting the physical requirements, potential donors must undergo thorough medical evaluations, including blood tests, imaging, and psychological assessments. These tests help determine if the individual is physically and mentally prepared for the demands of a Living Donor Transplant. Only those who meet all these criteria can safely proceed with the surgery, ensuring the best possible outcome for both the donor and the recipient.
In a Living Donor Transplant, ensuring that the donor and recipient have compatible blood groups is crucial for a successful procedure. The compatibility between the donor’s and recipient’s blood types helps minimize the risk of rejection, where the recipient’s immune system attacks the transplanted liver. Blood group compatibility is similar to what’s required for blood transfusions, where matching blood types prevent adverse reactions.
Here’s how blood group compatibility typically works in living liver donation:
While blood group compatibility is important, advancements in medicine have allowed for certain cases where incompatible blood types may still result in a successful transplant. Specialized medical procedures like plasmapheresis may be used in these scenarios to reduce the risk of rejection.
For both the liver donor and recipient, careful blood group matching and pre-surgical tests are essential to ensure the highest chances of success in the Living Donor Transplant process.
Becoming a part of a living liver donation is a profoundly impactful decision that can save lives. There are numerous advantages for both the donor and the recipient when choosing a Living Donor Transplant over a traditional deceased donor transplant.
For the recipient, one of the most significant benefits is the reduced waiting time. Patients suffering from liver failure often face long waitlists for a suitable deceased donor. With a Living Donor Transplant, the transplant can be scheduled much sooner, significantly improving the patient’s chances of recovery.
Additionally, the donated liver portion from a living donor is generally healthier, as it comes from someone in good health rather than a deceased individual. This can lead to better transplant outcomes for the recipient.
Key benefits of liver donation include:
In short, living liver donation offers hope and quicker recovery for patients, while donors experience the deep satisfaction of giving someone a second chance at life.
While a Living Donor Transplant offers many benefits, it also comes with important risks and considerations that both the donor and recipient should carefully evaluate. Donating a portion of your liver is a major decision, and the process involves thorough medical and psychological assessments to ensure it is safe for both parties involved.
The key risks associated with a living liver donation include:
Key considerations for donors include:
A Living Donor Transplant can be an emotionally fulfilling process, but it is crucial for potential donors to understand all risks and have realistic expectations about the recovery and impact on their lifestyle.
Before undergoing a Living Donor Transplant, both the donor and recipient must go through a comprehensive preparation and evaluation process. This stage is critical to ensure the safety and success of the procedure for both parties.
The potential liver donor will undergo a series of medical, psychological, and physical assessments to confirm their suitability for the transplant. This evaluation ensures that the donor is in optimal health and fully prepared for the surgery. The recipient will also be assessed to determine their readiness for receiving a new liver.
Key steps in the preparation and evaluation process include:
For the recipient, the evaluation ensures they are physically prepared to handle the transplant and the post-surgery recovery process. Both parties need to be fully informed about the living liver donation process, risks, and long-term care. Proper preparation and evaluation are essential for a successful liver transplant surgery.
The Living Donor Transplant surgical procedure is a highly specialized and carefully planned process that involves both the donor and the recipient. The procedure typically lasts between 6 to 8 hours and requires a skilled surgical team to ensure a successful outcome. The liver has a unique regenerative ability, which makes living liver donation possible.
Here’s how the surgical procedure generally unfolds:
The key benefits of this approach include:
However, like any major surgery, there are risks involved, including infection and complications related to anesthesia. Despite these risks, Living Donor Transplant is a life-saving option that significantly improves the patient’s survival chances.
Partial liver donation plays a vital role in living donor liver transplants, offering a life-saving alternative for those suffering from liver failure. In this procedure, the donor donates a portion of their liver, usually the left or right lobe, tailored to the recipient's size and medical needs. The remaining liver in the donor regenerates to its full size within weeks, ensuring both donor and recipient can achieve normal liver function. This remarkable regenerative capacity of the liver allows for quicker recovery and reduces the risks associated with waiting for a deceased donor liver.
Benefits of Partial Liver Donation:
Recovery and follow-up are crucial stages after a Living Donor Transplant for both the donor and recipient. While the procedure itself is life-saving, the post-surgery period requires careful attention and medical supervision to ensure successful outcomes.
For the liver donor, recovery typically involves:
Key aspects of liver donor recovery include:
For the recipient, the recovery process is longer, with close medical supervision required for months after the Living Donor Transplant. Regular follow-up appointments ensure the transplanted liver functions correctly, and any signs of rejection or infection are promptly addressed. Successful recovery often leads to significant improvements in the recipient's quality of life.
Living donor liver transplant offers a life-saving option for patients suffering from liver failure. By using a partial liver from a healthy donor, this procedure significantly reduces waiting times, allowing recipients to receive the care they need more promptly. Both the donor and recipient benefit from the liver's remarkable ability to regenerate, ensuring a full recovery for both. A living donor liver transplant not only saves lives but also enhances recovery outcomes, making it a preferred option in liver transplant care.
Yes, a living donor can donate a portion of their liver. Since the liver can regenerate, the donor’s liver will grow back to its original size within a few months after surgery, allowing them to lead a healthy life.
To be a living liver donor, a person must be in good physical and mental health, typically aged between 18 and 60, with a healthy body mass index (BMI), and no history of liver disease or serious conditions such as cancer, heart disease, or diabetes.
While there are risks associated with any surgery, liver donation is generally safe. The majority of donors recover fully within a few months. However, potential risks include infection, bleeding, and complications from anesthesia, which are closely monitored by the medical team.
Being a living liver donor saves a life and reduces the recipient’s wait time for a transplant. The donor’s liver regenerates, and many donors find great personal satisfaction in knowing they’ve made a life-changing impact on someone’s health.
The typical recovery time for a living liver donor is about 6 to 8 weeks. During this period, donors can return to light activities after a few weeks but are advised to avoid heavy lifting and strenuous exercise until fully healed, usually within three months. Regular check-ups ensure proper recovery.
Yes, a partial liver transplant can be performed using a live donor. In this procedure, the donor provides part of their liver, which is transplanted into the recipient. The donor’s liver regenerates within a few months, and the recipient’s new liver also grows to match their body’s needs, restoring normal liver function.
Yes, partial liver transplants are highly successful. Both the donor’s liver and the recipient’s transplanted liver regenerate over time, allowing them to regain full liver function. Success rates are high, especially when performed at specialized centers with experienced transplant teams, making partial liver transplants a viable and life-saving option for many patients.

Fatty liver disease, once a rare condition, has now become
Cirrhosis of the liver is a serious medical condition that




Undergoing a liver transplant is a monumental step in treating

A liver transplant is a crucial and intricate surgical procedure

Embarking on a liver transplant journey in India is a
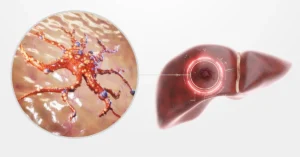
Liver cancer is a serious and life-threatening condition that affects thousands of people worldwide. With early detection and proper treatment, there is hope for managing and even overcoming this disease. We will delve into the complexities of liver cancer, exploring its definition, types, symptoms, causes, treatment options, and prevention methods.
Cirrhosis of the liver is a serious medical condition that affects millions of people worldwide. Understanding this disease, its causes, symptoms, stages, and available treatments can help manage and potentially prevent its progression.

A Deceased Donor Transplant, specifically a cadaveric liver transplant, is a life-saving procedure for individuals suffering from severe liver disease.

Liver transplants in India have become a crucial procedure for patients with severe liver conditions. As this life-saving surgery gains prevalence, it’s important to understand the legal and ethical considerations guiding the process.