Acute Rejection Episodes
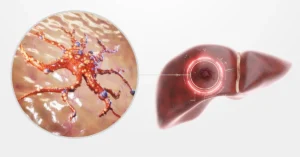
Acute rejection episodes are a significant concern following a liver transplant. This complication occurs when the body’s immune system mistakenly identifies the new liver as a foreign object and attacks it. Early detection and management of acute rejection are crucial to ensuring the success of liver transplant surgery.
- Definition and Causes: Acute rejection is an immune response that can happen days to weeks after a liver transplant. It is triggered by the body’s natural tendency to reject unfamiliar tissue, including the newly transplanted liver. Factors contributing to acute rejection include genetic differences between the donor and recipient and variations in the immunosuppressive regimen.
- Symptoms: Patients may experience symptoms such as fever, abdominal pain, jaundice (yellowing of the skin and eyes), and dark urine. These signs are indicative of the liver’s compromised function and require prompt medical attention.
- Diagnosis: Diagnosis typically involves a combination of blood tests to check liver function and liver biopsy to confirm rejection. The biopsy helps determine the extent of rejection and guides treatment decisions.
- Treatment: Treatment for acute rejection involves increasing the dosage of immunosuppressive medications, such as corticosteroids, to suppress the immune response. In some cases, additional medications may be required to manage the condition effectively.
- Prognosis and Follow-Up: With timely treatment, most episodes of acute rejection can be managed successfully, and liver function can be restored. Regular follow-up visits are essential to monitor liver health and prevent future rejection episodes.
Understanding and managing acute rejection is critical for successful liver transplant recovery and long-term health.
Chronic Rejection and Long-Term Monitoring
Chronic rejection is a significant concern for liver transplant recipients and requires careful long-term monitoring to ensure the continued health of the transplanted liver. Unlike acute rejection, which occurs shortly after the surgery, chronic rejection develops gradually over months or even years. This ongoing immune response can lead to the progressive loss of liver function, making vigilant monitoring and management crucial for the success of liver transplant surgery.
- Progressive Symptoms: Chronic rejection often presents with subtle symptoms such as persistent fatigue, weight loss, and jaundice. Patients may experience a gradual decline in their overall health, which makes routine check-ups essential for early detection.
- Regular Liver Function Tests: Long-term monitoring involves frequent liver function tests to detect any signs of chronic rejection. These tests help assess the liver’s ability to perform its critical functions and guide necessary adjustments in the treatment plan.
- Immunosuppressive Therapy Adjustment: Management of chronic rejection often requires adjustments to immunosuppressive medications. These medications are crucial in preventing the immune system from attacking the transplanted liver but must be carefully balanced to avoid potential side effects.
- Imaging and Biopsy: Periodic imaging studies and liver biopsies may be necessary to evaluate the condition of the transplanted liver and identify any chronic damage. These diagnostic tools provide detailed insights into liver health and aid in tailoring treatment strategies.
- Patient Education and Support: Educating patients about the signs of chronic rejection and the importance of adherence to follow-up appointments is vital. Support systems, including regular consultations with healthcare providers, help manage expectations and maintain optimal liver function.
Effective management of chronic rejection and vigilant long-term monitoring are integral to ensuring the success of liver transplant recovery and maintaining overall health.
Liver Dysfunction and Biliary Complications
Liver dysfunction and biliary complications are significant concerns after a liver transplant, impacting the overall success of the procedure and the patient’s quality of life. Understanding these issues and their management is crucial for a successful liver transplant recovery.
Liver dysfunction occurs when the transplanted liver does not perform its expected functions, such as detoxifying the blood and producing essential proteins. This dysfunction can be due to a variety of reasons, including graft rejection, infection, or complications from the transplant surgery itself. Symptoms of liver dysfunction may include jaundice (yellowing of the skin and eyes), abdominal pain, and fatigue. Monitoring liver function through regular blood tests is essential for early detection and intervention.
Biliary complications involve issues with the bile ducts, which can significantly affect liver function. These complications include:
- Bile Duct Strictures: Narrowing of the bile ducts that can obstruct bile flow, causing pain and jaundice.
- Bile Leaks: Leakage of bile from the bile ducts into the abdominal cavity, which can lead to infections and other complications.
- Biliary Infections: Infections in the bile ducts that can cause fever and discomfort.
- Cholestasis: A condition where bile flow is reduced or stopped, leading to bile buildup in the liver and potentially causing damage.
- Stone Formation: Formation of stones in the bile ducts that can block bile flow and cause pain.
Management of these complications often involves imaging techniques like ultrasound or MRI to diagnose the issue, and treatments such as endoscopic procedures or surgical interventions to correct the problems. Regular follow-up with healthcare providers is essential to address these issues promptly and maintain optimal liver function post-transplant.
Medication Side Effects and Management
After a liver transplant, managing medication side effects is a crucial aspect of ensuring a successful recovery. Post-transplant medications, particularly immunosuppressants, are essential to prevent organ rejection, but they come with their own set of challenges. Here’s a detailed look at common side effects and strategies for managing them effectively:
- Infections: Immunosuppressants can weaken the immune system, making patients more susceptible to infections. Regular monitoring and prophylactic treatments are essential to manage this risk. Patients should be vigilant about signs of infection and report them promptly to their healthcare provider.
- Diabetes: Medications such as corticosteroids can lead to glucose intolerance or diabetes. Patients need to monitor their blood sugar levels regularly and follow a diet and lifestyle plan to manage this risk. Medication adjustments may also be necessary.
- Hypertension: Some immunosuppressive drugs can cause high blood pressure. Regular blood pressure checks and lifestyle modifications, such as reducing salt intake and increasing physical activity, can help manage hypertension.
- Kidney Dysfunction: Long-term use of certain immunosuppressants can affect kidney function. Monitoring kidney function through regular blood tests and adjusting medication dosages are crucial for managing this side effect.
- Gastrointestinal Issues: Nausea, vomiting, and diarrhea are common side effects of post-transplant medications. These can often be managed with dietary adjustments and medications to alleviate symptoms.
Effective management of these side effects involves a combination of regular medical check-ups, lifestyle adjustments, and open communication with healthcare providers to tailor the medication regimen to the patient’s needs. By addressing these issues proactively, patients can improve their quality of life and support their long-term recovery after liver transplant surgery.
Psychosocial Impact and Support Systems
The psychosocial impact of a liver transplant can be profound, affecting not only the patient’s emotional well-being but also their overall quality of life. The journey through liver transplant surgery is fraught with emotional and psychological challenges that can persist long after the operation. Recognizing and addressing these issues is crucial for a successful recovery and long-term health.
Psychosocial Impact
- Emotional Distress: Patients often face anxiety, depression, and stress as they adjust to their new lifestyle and manage the complexities of post-transplant care.
- Body Image and Self-Esteem: The physical changes and ongoing medical treatments can affect self-image and confidence.
- Lifestyle Changes: Adapting to new medications, dietary restrictions, and frequent medical appointments can be overwhelming.
Support Systems
- Family Support: Emotional support from family members is vital. Family members can help patients cope with the stress and provide practical assistance during recovery.
- Professional Counseling: Engaging with mental health professionals can help manage anxiety and depression. Therapy can offer coping strategies and emotional support.
- Support Groups: Joining liver transplant support groups allows patients to connect with others who have had similar experiences, providing a sense of community and shared understanding.
- Patient Education: Educating patients about the transplant process and recovery can reduce anxiety and improve confidence in managing their health.
- Social Services: Accessing social services for additional support, such as financial assistance and transportation, can ease the burden of recovery.
By addressing these psychosocial impacts and leveraging support systems, patients can better navigate the challenges of liver transplant recovery and improve their overall well-being.